Mitochondrial Dysfunction in Autism: Testing & Treatments

All contents of this resource were created for informational purposes only and are not intended to be a substitute for professional advice, diagnosis, or treatment. Always seek the advice of your physician, therapist, or other qualified health providers with any questions or concerns you may have.
Suzanne Goh, MD
One of the most exciting areas of research in autism spectrum disorder (ASD) is in the role of mitochondrial function. Research studies looking at mitochondrial function in those with autism are transforming the way we think about the causes of autism and are pointing to medical therapies that could have a significant impact. This article will address the role of mitochondria in autism and the diagnosis and treatment of mitochondrial dysfunction.
What are Mitochondria?
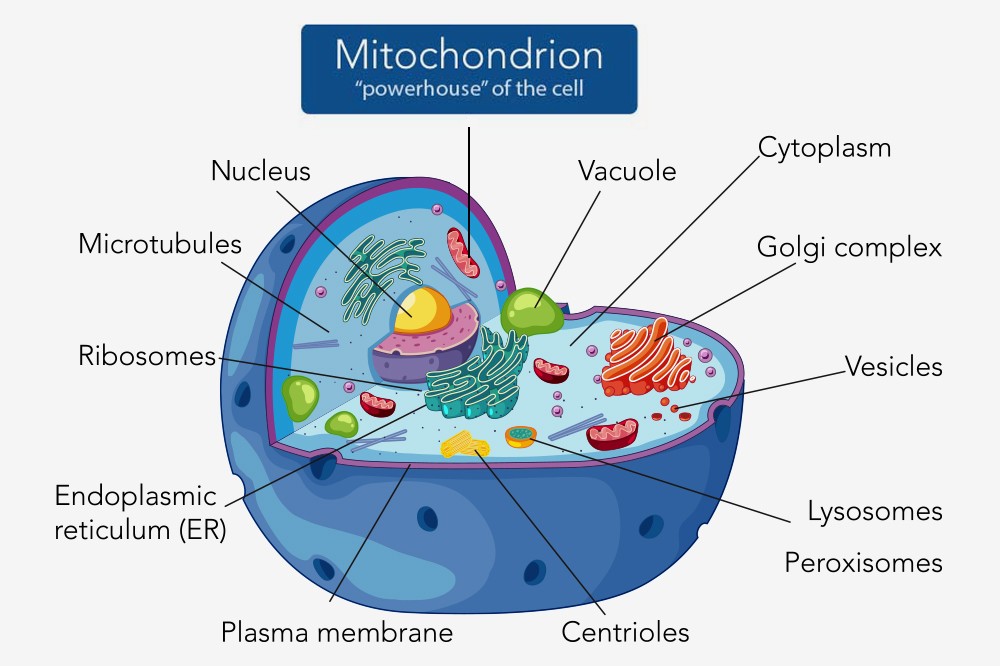
Mitochondria are tiny structures located within nearly all cells of the body. They are the parts of the cell that are primarily responsible for creating energy. They do this by generating adenosine triphosphate (ATP), which is the essential “fuel” that drives all of the body’s functions. For this reason, mitochondria are often described as the “powerhouse” of the cell.
A single cell can have up to several thousands of mitochondria. Cells of the brain and muscle are among those that require a lot of energy, so they have a particularly high density of mitochondria to support their energy needs. When mitochondria aren’t working well, these are often the parts of the body to show signs of poor function.
Symptoms of Mitochondrial Dysfunction
When mitochondria are not functioning well, a wide variety of symptoms can emerge, including:
- Developmental delay or regression
- Language impairment
- Social impairment
- Intellectual disability
- Neuropsychiatric symptoms (ADHD, anxiety, OCD, depression)
- Seizures
- Headaches
- Hearing impairment
- Weakness
- Small stature
- Fatigue
- Gastrointestinal symptoms
- Endocrine disturbance
- and many others
More and more research now suggests that mitochondrial dysfunction may be important in many different health conditions:
- Autism
- Bipolar disorder
- Schizophrenia
- Depression
- Diabetes
- Parkinson’s disease
- Asthma
- Chronic fatigue syndrome
- Alzheimer’s disease
- A variety of gastrointestinal disorders
- And others…
Mitochondrial Dysfunction and Autism Spectrum Disorder

Research in mitochondrial dysfunction in ASD has grown in recent years, and there are now many research studies linking mitochondrial dysfunction to ASD.
In 2010, a groundbreaking study by researchers at University of California Davis showed that 80% of the children with ASD enrolled in their study had blood tests indicating mitochondrial dysfunction (1).
Other research studies have found
- Biochemical evidence of mitochondrial dysfunction in post-mortem brain tissue of children and adults with ASD (2, 3)
- Markers of mitochondrial dysfunction on brain MR spectroscopy scans of children and adults with ASD (4)
- Mitochondrial and immune abnormalities in children with ASD (5, 6)
The cumulative evidence now suggests that mitochondrial dysfunction is present in a substantial portion of those with ASD and that it may be an important factor that contributes to the symptoms of ASD.
Triggers of Mitochondrial Dysfunction in Autism
Many different types of triggers can lead to mitochondrial dysfunction, and these may be either genetic or environmental, or a combination of both. Some of the triggers include
- gene mutations,
- shortages of key vitamins and minerals in the diet,
- certain chemicals, heavy metals, and drugs,
- certain bacteria and viruses,
- stress
Mitochondrial dysfunction, therefore, is a potential explanation for how different types of environmental insults might lead to the symptoms of ASD. One theory is that certain environmental insults may affect those with ASD because they already have an underlying genetic vulnerability that, when combined with an environmental insult, can lead to the symptoms of ASD.
Diagnosis of Mitochondrial Dysfunction in Autism
There are many different tests that can be done to look for signs of mitochondrial dysfunction. Some common first-line tests include
- Blood testing: Complete metabolic profile (Chem 20), lactate, pyruvate, amino acids, creatine kinase, ammonia, total and free carnitine, acylcarnitine profile
- Urine testing: organic acids
Brain imaging using magnetic resonance spectroscopy (MRS) may show elevated lactate (which is a biomarker of mitochondrial dysfunction). Information on mitochondrial function can also be obtained through a test called MitoSwab which requires only a cheek swab and can provide information on mitochondrial enzyme function.
When testing for mitochondrial dysfunction, it is important to keep in mind that many of the available tests have low sensitivity – meaning that the results may appear normal even if an individual has mitochondrial dysfunction. Testing may need to be repeated multiple times or may need to be done during specific physiological conditions, such as during fasting or during illness. Because of these challenges, a physician may recommend treatment even if test results are negative, especially if there are aspects of the individual’s medical history that suggest mitochondrial dysfunction is present.
Some of the features of the medical history that would raise a “red flag” for mitochondrial dysfunction include:
- Developmental plateau or regression, especially in the setting of illness or other physiological stress
- Symptoms in more than one organ system
- Family members with diseases that have been linked to mitochondrial dysfunction
- Alzheimer’s disease, Parkinson’s disease, Huntington Disease, Lou Gehrig’s disease (ALS), intellectual disability, deafness, blindness, stroke, migraine headaches
- Diabetes, obesity, cardiovascular disease
- Multiple sclerosis, lupus, rheumatoid arthritis
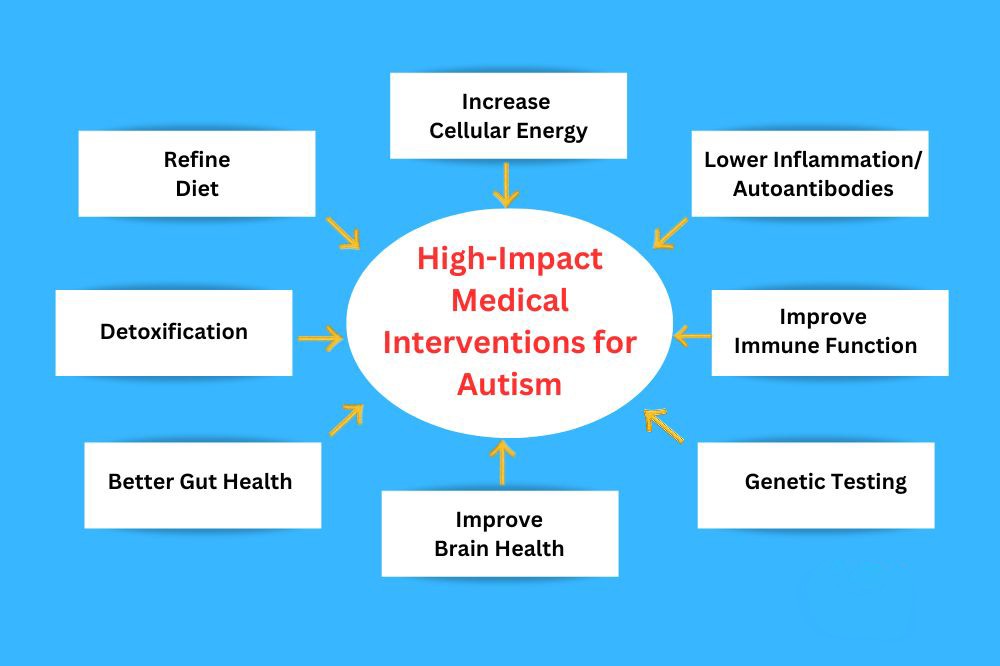
Treatment Approach for Mitochondrial Dysfunction

Physicians may recommend several steps for supporting mitochondrial function. These include
- Limiting periods of fasting, increasing meal frequency, and improving hydration
- Avoiding mitochondrial toxins (e.g., Valproic acid, certain cholesterol-lowering medications, aminoglycoside antibiotics, acetaminophen, metformin, beta-blockers, etc.)
- Avoiding physiologic stressors when possible (e.g., illness, dehydration, fever, temperature extremes, surgery, anesthesia, prolonged fasting or starvation) especially in combination
- Providing supportive care during conditions of physiologic stress (e.g., hydration, nutrition, L-carnitine, CoQ10, Vitamin C & E, L-arginine)
- Consistent, moderate exercise
Certain vitamins and supplements also may be recommended (and should be used under the supervision of a physician) (7):
- L-carnitine – a compound required for the transport of certain fatty acids into the mitochondria so they can be oxidized (“burned”) to produce energy. Carnitine is generated in the liver and kidneys from the amino acids lysine and methionine. Some individuals cannot make enough carnitine and are dependent on supplementation through the diet.
- Coenzyme Q10 – a natural antioxidant that is synthesized in the body and found in many foods. It functions both as an antioxidant and also as a key participant in the mitochondrial respiratory chain.
- Vitamin C – a water-soluble vitamin that is naturally present in many foods. Vitamin C is an important physiological antioxidant and has been shown to regenerate other antioxidants in the body, including vitamin E. It helps to counter the damaging effects of free radicals on cellular and mitochondrial function.
- Vitamin E – a fat-soluble vitamin that comes in many different chemical forms. Alpha-tocopherol is the form of vitamin E that is most widely recognized to meet human requirements and is the form most commonly found in supplements. Vitamin E is a potent antioxidant and helps to protect cells from the damaging effects of free radicals.
- Vitamin B1 (thiamine) – a water-soluble B-complex vitamin that must be consumed in the diet. Vitamin B1 is involved in numerous metabolic processes and a deficiency can cause severe neurological symptoms including delirium, neuropathy, and sleep disturbance.
- Vitamin B2 (riboflavin) – a water-soluble B-complex vitamin that is essential to many enzymatic reactions that take place in the mitochondria. Sources of Vitamin B2 include milk, cheese, leafy vegetables, mushrooms, and almonds.
- Vitamin B3 (niacin or niacinamide) – a water-soluble B-complex vitamin that, if deficient, can lead to symptoms such as nausea, anemia, headaches, and fatigue.
- Vitamin B5 (pantothenate) – a water-soluble B-complex vitamin that is needed in order to synthesize coenzyme-A which is important in the synthesis and oxidation of fatty acids and in the Krebs cycle.
- Vitamin B7 (biotin) – a water-soluble vitamin that is necessary for cell growth and the metabolism of fats and amino acids.
- Vitamin B9 (folate) – a water-soluble vitamin that is essential for many bodily functions and must be supplied through the diet. Folate is important in the synthesis, repair, and methylation of DNA and is a cofactor in many biological reactions. Folate deficiency has been linked to neurological defects in the developing embryo.
- Vitamin B12 (cobalamin) – a water-soluble vitamin with a key role in the normal functioning of the brain and entire nervous system. Vitamin B12 plays an important role in DNA synthesis and regulation as well as fatty acid metabolism and amino acid metabolism.
- L-Creatine – an organic acid that facilitates the formation of adenosine triophosphate (ATP) and thereby helps to supply energy to all of the cells of the body, and in particular to muscle. Creatine is made in the body and is also consumed in the diet (mainly from meat products).
- Alpha Lipoic Acid – a compound that is important in many different aspects of aerobic metabolism including the Krebs cycle.
- L-Arginine – an amino acid that is produced in the body but also needs to be consumed through the diet to achieve sufficient amounts. L-arginine plays an important role in cell division, wound healing, detoxification, immune function, and hormone release.
- Selenium – a chemical element necessary for cellular function and a component of several antioxidant enzymes.
It is important to work with a physician in tailoring the right mitochondrial treatment protocol. The types of supplements that may be useful, their dosage, and the duration of treatment should all be managed by a qualified clinician. If not used correctly, some vitamins and supplements may have the potential for adverse effects.
Treatment Outcomes for Those with Autism and Mitochondrial Dysfunction
The efficacy of mitochondrial supplements in ASD has not yet been studied in large-scale clinical trials. However, one study looked at the efficacy of supplementation with L-carnitine in children with ASD over a period of three months and found that treatment led to improvement in the symptoms of autism and in muscle strength (8). The number of children studied was small, and future studies are needed in order to understand how mitochondrial supplements can best be used in the treatment of those with ASD.
The United Mitochondrial Disease Foundation provides this summary of the potential benefits of therapy:
- Sometimes, treatment may be beneficial and noted immediately
- Sometimes, the benefits of treatment may take a few months to notice
- Sometimes, the benefits of treatment may never be noticed, but the treatment may be effective in delaying or stopping the progression of the disease
- Sometimes, some patients may not benefit from therapy.
Additional Resources
For more information about mitochondrial dysfunction, go to:
- United Mitochondrial Disease Foundation
- MitoAction
- Mitochondrial Medicine Society
- Underlying Medical Issues in Autism
- Lab Testing
References
- Giulivi, et al., Mitochondrial Dysfunction in Autism. Journal of the American Medical Association. 2010;304:2389-2396.
- Chauhan, et al., Brain region-specific deficit in mitochondrial electron transport chain complexes in children with autism. Journal of Neurochemistry 2011;117:209-22.
- Tang, et al., Mitochondrial abnormalities in temporal lobe of autistic brain. Neurobiology of Disease 2013;54:349-361.
- Goh, et al. Mitochondrial Dysfunction as a Neurobiological Subtype of Autism Spectrum Disorder: Evidence from brain imaging. JAMA Psychiatry 2014; 71:665-671.
- Napoli, et al., Deficits in bioenergetics and impaired immune response in granulocytes from children with autism. Pediatrics 2014;133:e1405-10.
- Rose, et al., Oxidative stress induces mitochondrial dysfunction in a subset of autism lymphoblastoid cell lines in a well-matched case control cohort. PLOS One 2014;9:e85436.
- Parikh, et al. A Modern Approach to the Treatment of Mitochondrial Disease. Current Treatment Options in Neurology. 2009; 11: 414-430.
- Geier, et al. A prospective double-blind, randomized clinical trial of levocarnitine to treat autism spectrum disorders. Med Sci Monit 2011;17:PI15-23.